Cost effectiveness of smart insoles in preventing ulcer recurrence for people in diabetic foot remission
Clinical Evidence
ProvidersPayers
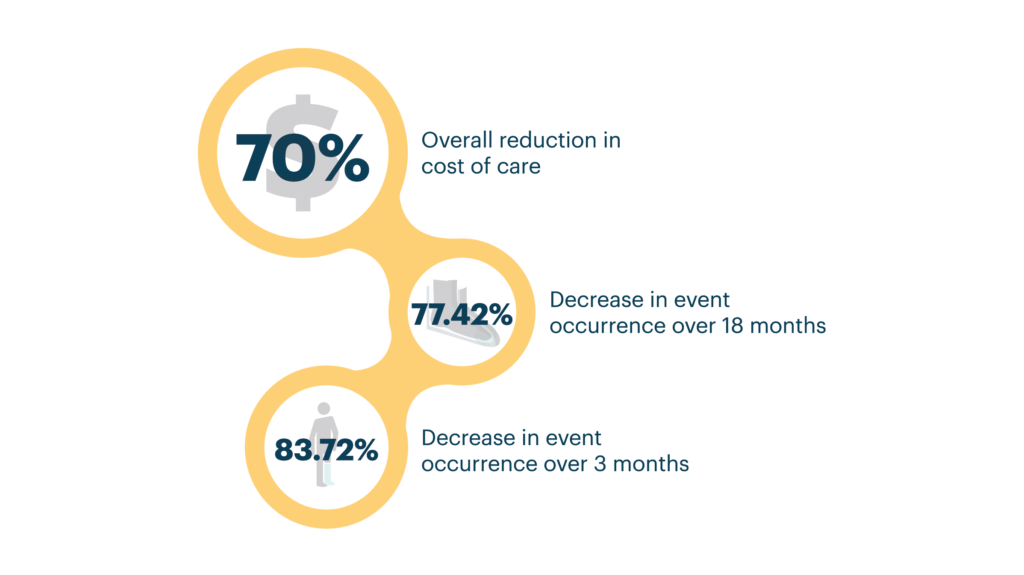
A peer-reviewed study showed a drastic decrease in the occurrence of foot ulcers and a substantial cost savings when using SOC + Orpyx technology
Abstract
AimsTo show that a device designed to prevent diabetic foot ulcers (DFUs) may help to cost-effectively manage patients at a high- risk of recidivism.
Methods
Decision tree models were used to estimate clinical outcome probabilities and associated costs at three- and 18-months post-DFU closure, comparing standard of care (SOC), or SurroSense Rx® as an adjunct to SOC. Inputs were derived from a prospective cohort study (n=15) involving patients with a recent (<12 months) history of DFU. This analysis was conducted from the third-party payer perspective with costs presented in 2017 USD.
Results
Short-term (three month) results show that care involving the adjunctive use of SurroSense Rx saves approximately US$978·02 per event avoided (excluding device costs) compared to SOC.
Long-term (18-month) results suggest lower event occurrence rates (0·14 versus 0·62), with a cost per ulcer avoided of US$6,702·54 (versus US$53,134·94 with SOC alone); this indicates the SurroSense Rx + SOC as the dominant strategy.
Conclusions
The results support the cost-effectiveness of smart insoles as an adjunct to diabetic foot care—this could result in substantial savings for the US Health System. More robust studies are required to verify these results, and determine population-level cost savings.
Clinical Evidence
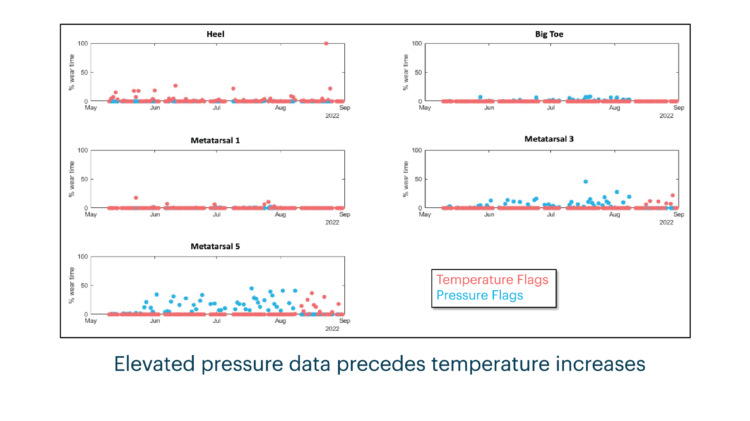
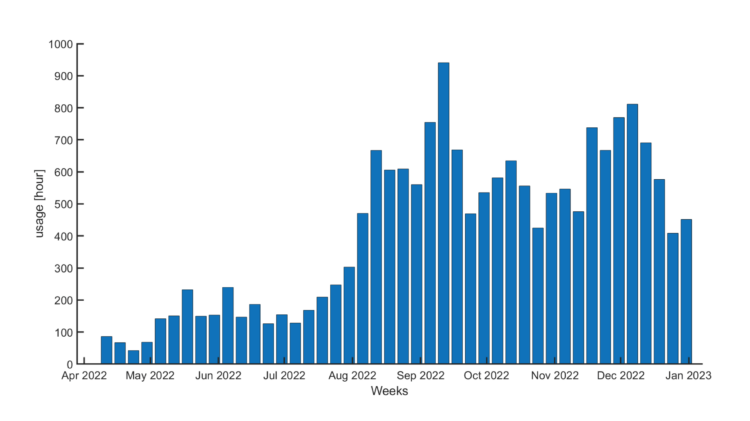
Preventative Sensor-Based Remote Monitoring of the Diabetic Foot in Clinical Practice

Clinical Evidence
Evaluating the Effectiveness of Plantar Sensory Insoles and Remote Patient Monitoring for Early Intervention in Diabetic Foot Ulcer Prevention in Patients with Peripheral Neuropathy
Clinical Evidence
Innovative Plantar Sensory Insoles To Prevent Foot Ulcer Recurrence and Guide Treatment Plans in Patients With Diabetic Peripheral Neuropathy